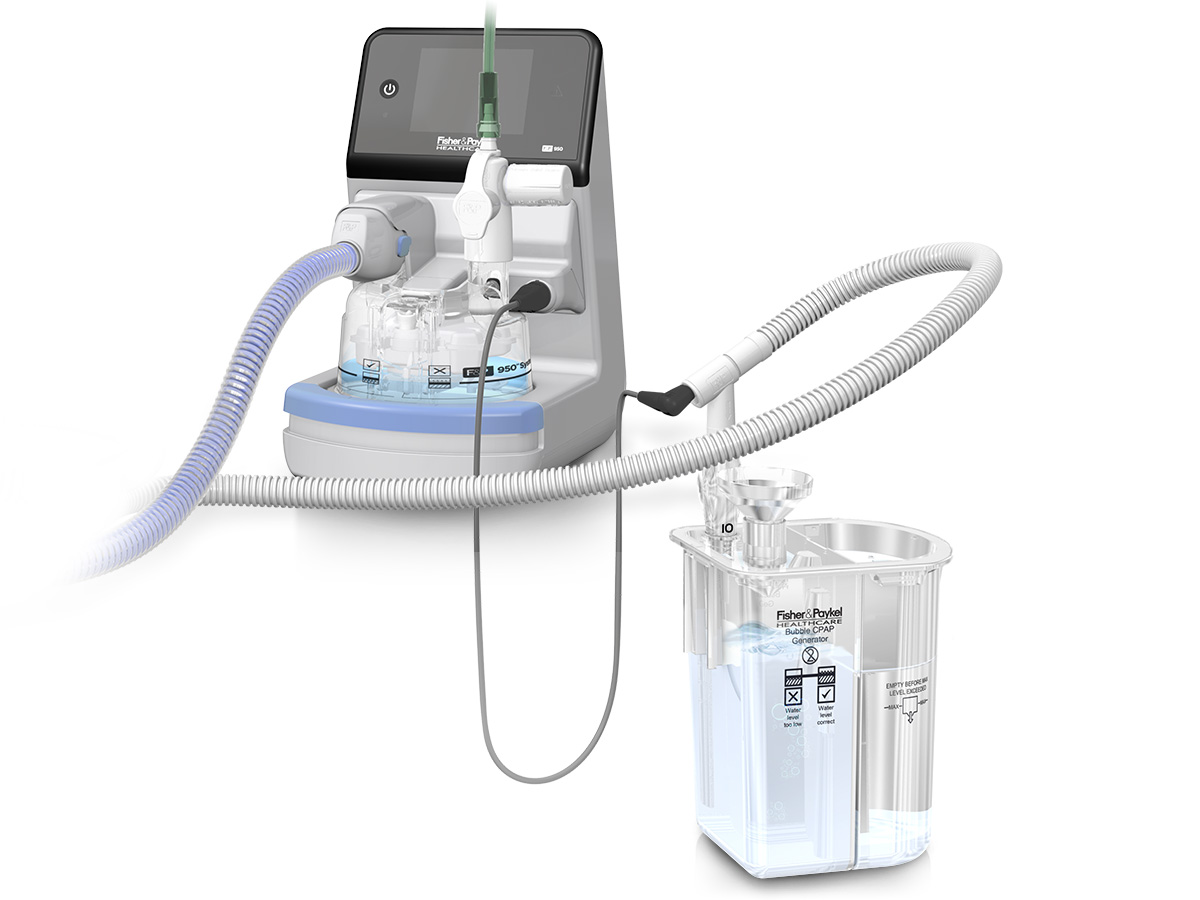
Bubble CPAP System
Designed to provide consistent pressure through an auto-leveling feature. The system includes circuits, a pressure-relief manifold and a Bubble CPAP generator.
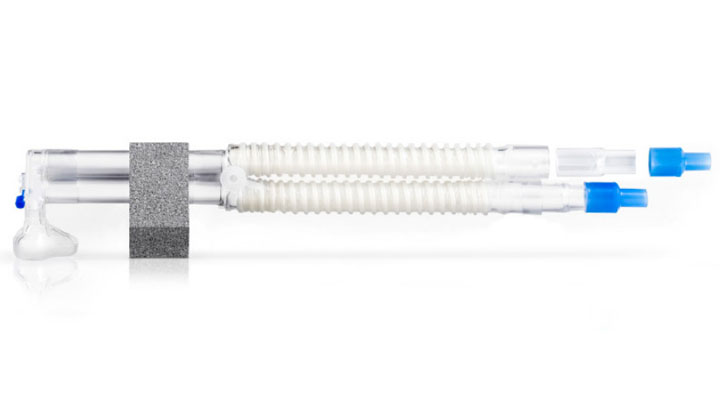
FlexiTrunk™ nasal CPAP interface
An integrated solution that includes all the components for delivering CPAP: nasal masks, nasal prongs, bonnets, and headgear. Provides a complete system when combined with a Bubble CPAP generator.
How does CPAP therapy work?
CPAP therapy delivers a mixture of heated, humidified air and oxygen and generates a continuous distending pressure throughout the respiratory cycle by means of a sealed interface.1,2
Selecting an appropriately-sized interface is important for achieving an adequate seal. Short bi-nasal prongs or a nasal mask are the most commonly used types of interfaces for delivering CPAP.3 The efficacy of delivered therapy is not impacted by the choice of prongs or mask (when using a true CPAP system) and the two can be cycled in clinical practice to alleviate contact points.4
Bubble CPAP, a mode of CPAP therapy, may offer an additional benefit to patients in that it generates pressure oscillations which may improve gas exchange and carbon dioxide (CO2) elimination.5 An underwater seal is created by submerging the expiratory tube in a variable depth of water. Gas exiting the expiratory tube produces bubbles that then generate pressure oscillations.1 CPAP can be used in both the acute and recovery phases of respiratory distress syndrome (RDS).6,7
There are several well-documented benefits and mechanisms of action associated with this therapy.
Maintains functional residual capacity (FRC)
CPAP enhances lung volume recruitment and helps establish and maintain adequate FRC (the volume of air that remains in the lungs following a typical expiratory phase).1,8,9 This volume is important for keeping the lungs open post exhalation.
CPAP has been shown to increase the volume of air remaining in the lungs after a typical expiratory phase, helping to keep the lungs open.1,8
As early as the 1970s, CPAP was shown to restore FRC, improve hypoxemia, reduce pulmonary vascular resistance and conserve surfactant.10,11
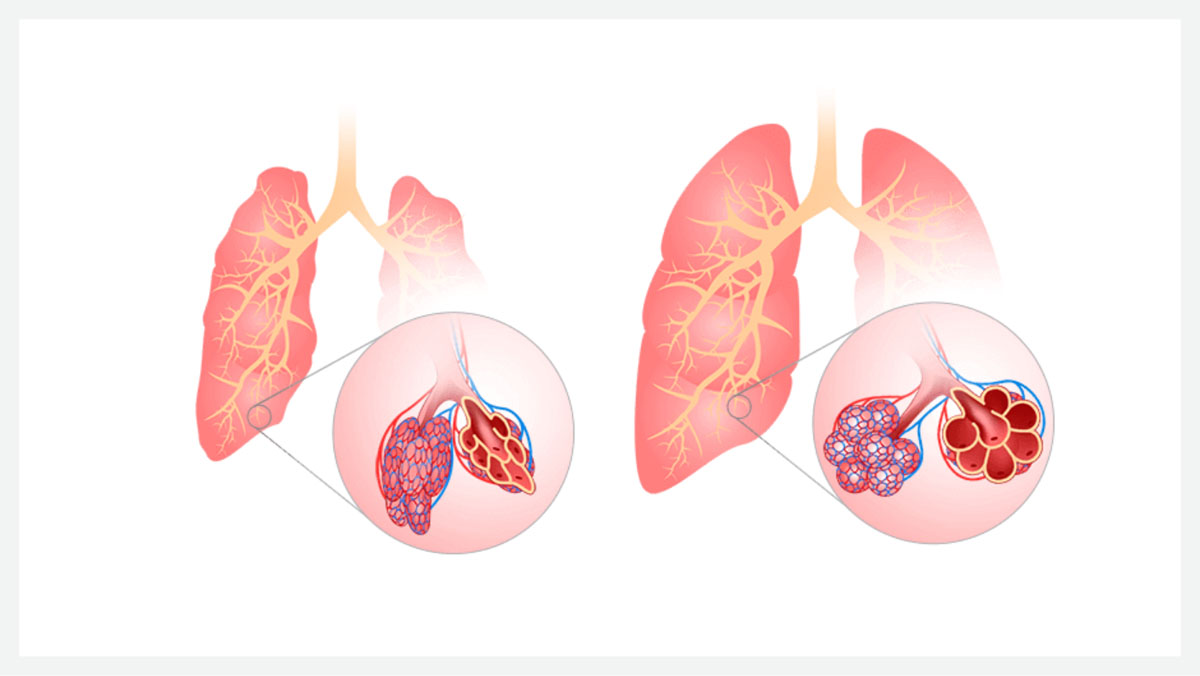
Fig 1. The impacts of CPAP on a neonatal lung under respiratory distress. Without positive airway pressure, FRC is decreased and resistance is high, resulting in alveolar collapse (pictured left). With the application of positive airway pressure (pictured right), FRC is maintained effectively and alveoli are held open.
Reduces the work of breathing
CPAP therapy can improve the work of breathing by reducing the energy required to expand the lungs for inspiration. 8,12,13
Work of breathing is the force required to expand the lungs against their elastic properties. CPAP has been shown to elevate end-expiratory lung volume, which helps to unload the inspiratory muscles and reduce the work of breathing. 8,12,13

Promotes airway hydration
During CPAP therapy, continuous distending pressure is generated throughout the respiratory cycle, and a heated and humidified mixture of air and oxygen is delivered.
Heated and humidified gas is an important aspect of delivering CPAP therapy, assisting with the natural defense mechanisms, maintaining airway mucosa and mucociliary function, and promoting conservation of energy for growth and development.24,25
Decreases the need for invasive ventilation
The use of CPAP alone, or CPAP in combination with a surfactant when used for primary respiratory support, has been associated with a reduced need for intubation and invasive ventilation.14,15
Invasive ventilation can be lifesaving, especially for preterm infants born less than 30 weeks’ gestation with respiratory distress syndrome (RDS). However, it may contribute to increased rates of chronic lung disease. The associated disadvantages of invasive ventilation have led to the development of more noninvasive ventilation strategies, including CPAP therapy.3 Research has shown that CPAP can be used as an alternative to routine intubation and invasive ventilation in neonates with RDS.16,17
Bubble CPAP generates pressure oscillations
Pressure oscillations generated during bubble CPAP therapy produce vibrations that are similar to those produced by high-frequency ventilation, and may improve gas exchange and CO2 elimination.5
Studies have demonstrated that these pressure oscillations may be transmitted down the airways and into the lungs.5,18
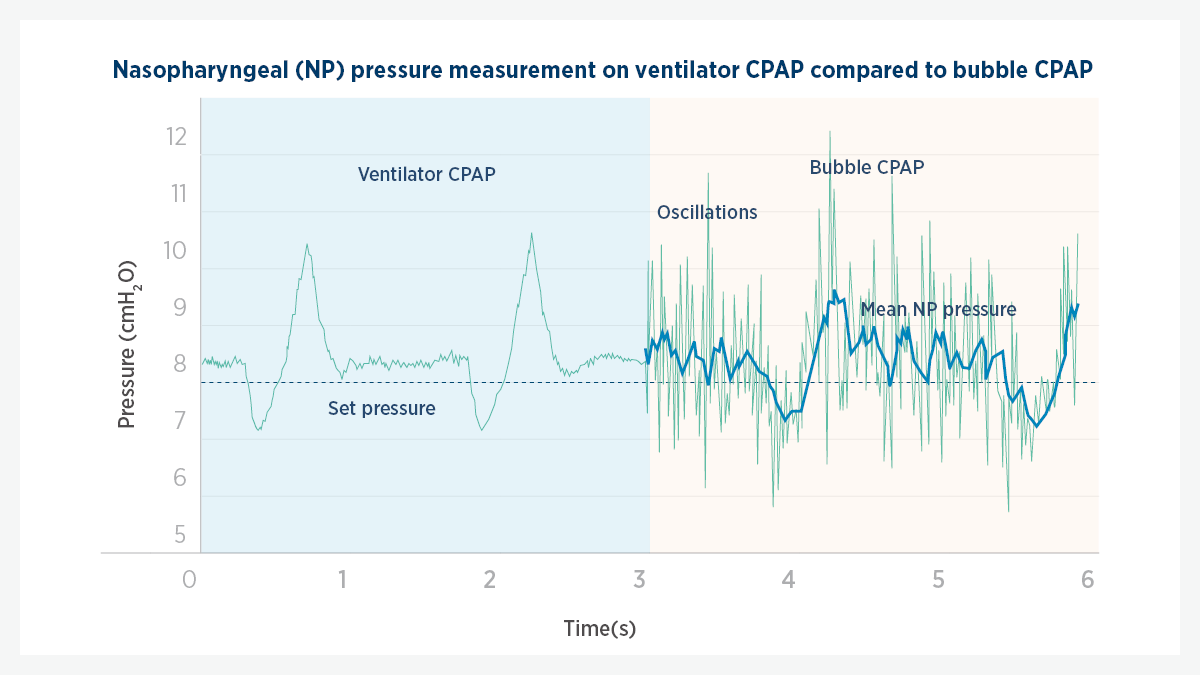
Fig 4. Graphical representation of bubble CPAP generated pressure oscillations. The pressure vs. time plot shows how pressure oscillations vary over time (green line) alongside the resulting mean airway/nasopharyngeal (NP) pressure (blue line).
CPAP can be used in neonates with RDS
Randomized controlled trials and systematic reviews have evaluated the use of CPAP as primary and postextubation respiratory support for premature and low-birth-weight neonates with RDS, both in the acute and recovery phases of this condition.3,6,7
In premature infants, RDS is the most common respiratory condition that CPAP has been used for since the 1970s.19,20 Several studies, which include randomized controlled trials and systematic reviews, have evaluated the use of CPAP as a mode of respiratory support in preterm neonates and infants with RDS and have concluded that CPAP is an effective mode of respiratory support for these patients. 3,14,21-23
.
The F&P Neonatal App is not intended to provide medical diagnoses or treatment advice. The app is intended exclusively for healthcare professionals and is not a substitute for the exercise of clinical judgment by an appropriately-qualified healthcare professional.
F&P and FlexiTrunk are trademarks of Fisher & Paykel Healthcare Limited. For patent information, see www.fphcare.com/ip
Apple and the Apple logo are trademarks of Apple Inc., registered in the U.S. and other countries. The App Store is a service mark of Apple Inc., in the U.S. and other countries. Google and Google Play are trademarks of Google LLC.