NHF therapy in practice in a children's hospital
Explore how the Queensland Children's Hospital uses NHF therapy across the hospital.

A non-sealing nasal interface specifically designed for the flow requirements and anatomical features of infants and children on NHF therapy.
How does NHF therapy work?
NHF is a flow-based therapy designed to be an open system that typically consists of a flow source to blend air and oxygen, a humidifier to heat and humidify the gas mixture, and a circuit and interface to deliver humidified gas to the patient. Suitable sizing of the nasal cannula is important to ensure the open system is maintained.
NHF is associated with a range of mechanisms of action and physiological benefits:
• Ensures washout of anatomical dead space.2-4
• Provides dynamic positive airway pressure.2-5
• Delivers heated and humidified gas.6-9
• Provides supplemental oxygen.10-12
• Improves patient comfort.13-16

Delivers heated and humidified gas
NHF delivers a heated and humidified blend of air and oxygen, maintaining the nasal mucosa and enhancing mucociliary function.6 It reduces mucosal dryness and improves secretion clearance compared with standard oxygen therapy.7 Consensus guidelines state that NHF should always be adequately heated and humidified.8,9
Provides supplemental oxygen
NHF differs from standard oxygen therapy in that it can accurately deliver a prescribed FiO2 when the set flow rate meets or exceeds a patient’s peak inspiratory demand.10,11
FiO2 is the proportion of oxygen in the air that is inspired.11 In addition to the ability to deliver accurate FiO2, the combined mechanisms of NHF have the effect of improving oxygenation status.10-12
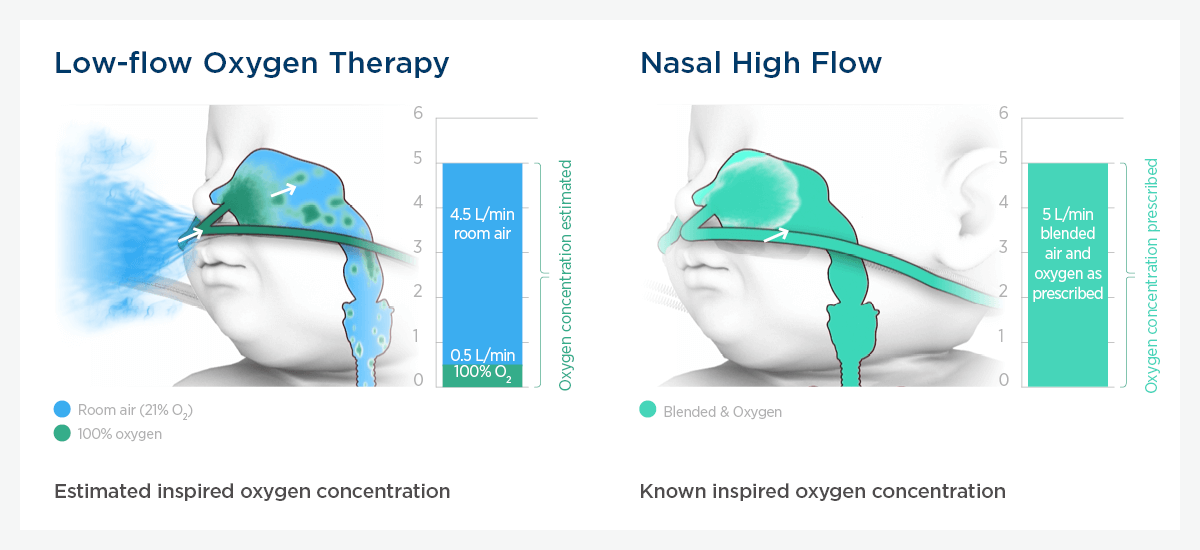
Compared with standard oxygen therapy, NHF can accurately deliver a prescribed FiO2 when set flow meets or exceeds the patient's peak inspiratory demand.

Improves patient comfort
Because NHF is an open system, it is gentle on the patient’s nose.
Compared with continuous positive airway pressure (CPAP), NHF improves patient comfort, compliance and tolerance to therapy.13,14 NHF is also associated with a significant reduction in the rate of nasal trauma.15,16
Clinical NHF studies have used objective measures, such as heart rate, facial expressions, and movement, to assess patient comfort.14
Updated March 2023
Optiflow Flow Matters
Early use of NHF in infants and children
In our pediatric edition of Optiflow™ Flow Matters, we review the literature and provide an evidence-based approach to the implementation of NHF in pediatric patients.
| Weight | Flow rate | Flows |
| Up to 12 kg | 2 L/kg/min | Up to 12 kg 2 L/kg/min for infants up to 12 kg in weight has been shown to produce rapid improvement in reducing respiratory distress, and a reduced need for the escalation of therapy. Over 12 kg Flow rates for those over 12 kg in weight have been protocolized by the PARIS research group.4 |
| 13 – 15 kg | 25 – 30 L/min | |
| 16 – 30 kg | 35 L/min | |
| 31 – 50 kg | 40 L/min | |
| > 50 kg | 50 L/min |
.
F&P and Optiflow are trademarks of Fisher & Paykel Healthcare Limited. For patent information, see www.fphcare.com/ip