Accelerate your understanding of the mechanisms of high flow therapy
If you want to be a high-flow pro, i.e., be able to identify which patients will benefit from high flow, knowing the mechanisms of action is the key!
It's a significantly more sophisticated form of respiratory support, that includes the provision of dynamic, positive airway pressure, and reduction of dead space.
The airway hydration resulting from heating and humidifying the air is critical to facilitating comfortable treatment but is equally valuable in preserving mucociliary function. This is why it's at the heart (or more accurately lungs) of this therapy.
As with any treatment, patient comfort is a significant factor. One of the standout features of NHF is the level of respiratory support that can be achieved without the downsides of a mask.
If you want to be a high-flow pro, i.e., be able to identify which patients will benefit from high flow, knowing the mechanisms of action is the key!
1.
Watch this F&P Micro Moment - How does NHF work?
Learn about the key mechanisms of action for nasal high flow, driven by flow and humidification.
(2 mins)
3.
Mechanisms in action
Step through each mechanism to see the science that underpins it - watch microscopic cilia beating, lungs expanding, dead space being cleared.
This short video explains the key mechanisms of action of Nasal High Flow, driven by flow and humidification.
Click here to see the full series of Micro Moments. #makeyourflowmatter
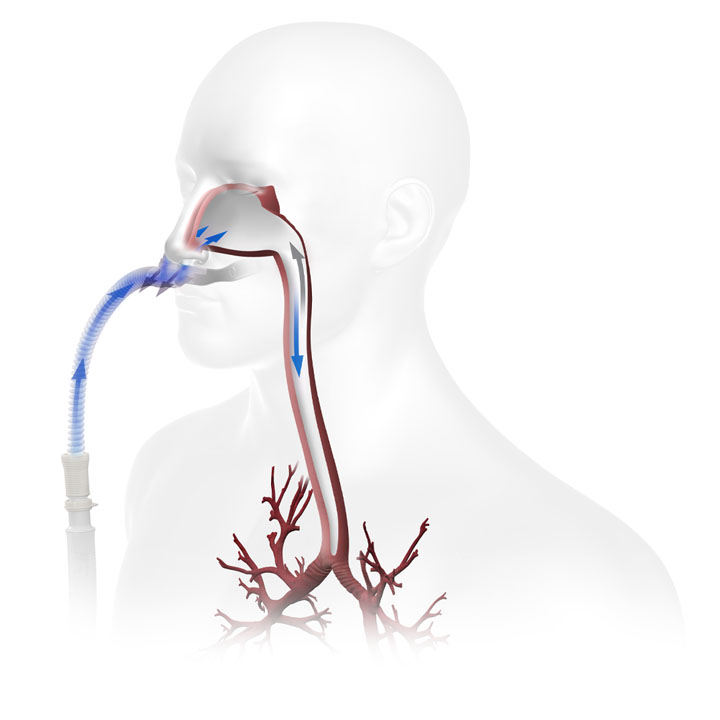
How dead space clearance improves oxygenation with just room air.
Watch this effect in action
(no audio)
This video depicts the clearance of a radioactive tracer from an upper airway model using Gamma camera imaging superimposed on a CT scan.
Flow rates were 15, 30, and 45 L/min.
In this experiment, as the flow rate increases, so does clearance.1
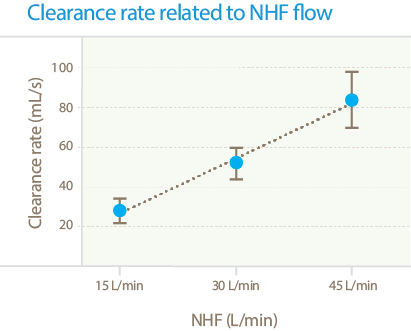
This effect is flow dependent2
NHF creates breath and flow-dependent pressure, making inspiration easier and promoting slow, deep breathing on expiration, thereby increasing alveolar ventilation.
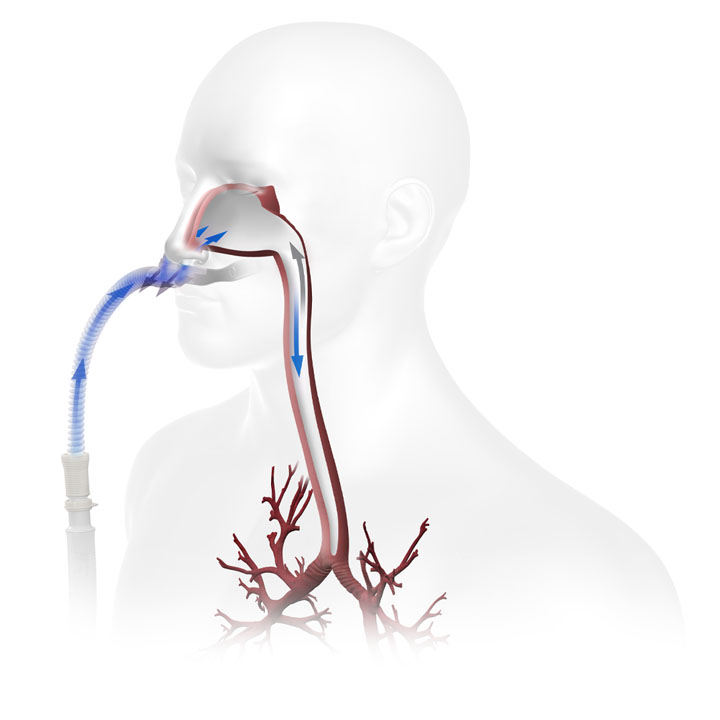
How pressure creates slower, deeper, more regular breathing.
Breath and flow-dependent airway pressure,2,3 ...
...promotes slower, deeper breathing by prolonging expiration time3 resulting in...
...an increase in alveolar ventilation3 and reduced work of breathing.
Watch this effect in action
(no audio)
Corley et al. 20114 demonstrated a significant increase in lung aeration once therapy starts.
This change reflects enhanced lung volume and tidal volume.
This effect is flow-dependent
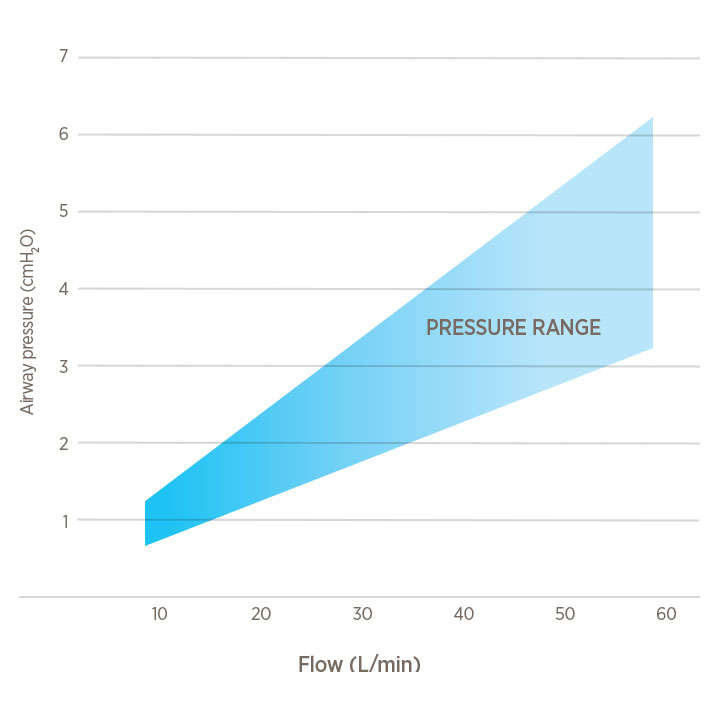
Increases approximately 0.5 - 1 cmH2O per 10 L/min3,5-6
Mean airway pressure (for illustrative purposes only)
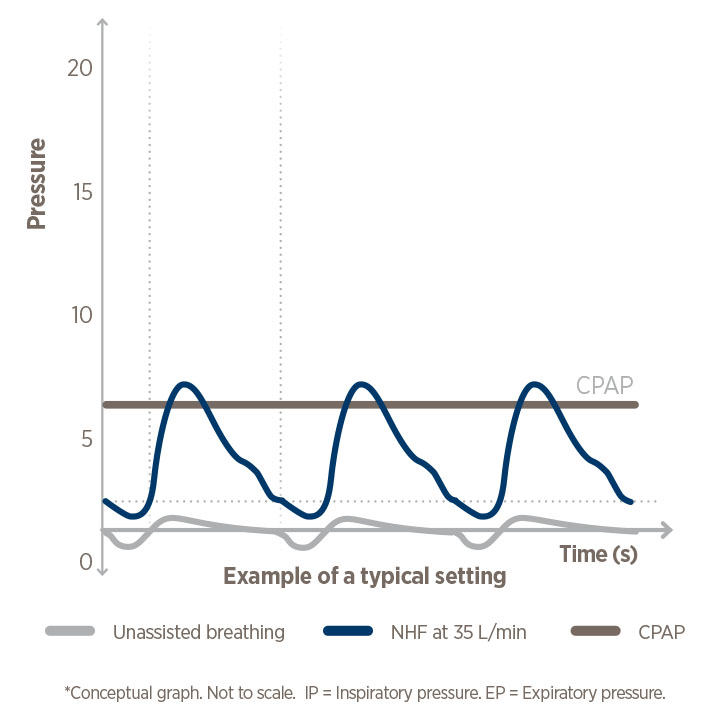
It's different from CPAP pressure!
NHF pressure is dynamic, not set, and not constant.
With NHF, the level of pressure changes throughout the breath cycle and is dependent on the size of cannula prongs, breathing rate, mouth opened or closed, i.e., pressure fluctuates.
Is the Airvo 2 a continuous positive airway pressure (CPAP) device?
Humidity...
...prevents desiccation of the airway epithelium7and...
...maintains9 and improves mucociliary clearance / transport7,8 as illustrated in the animation.
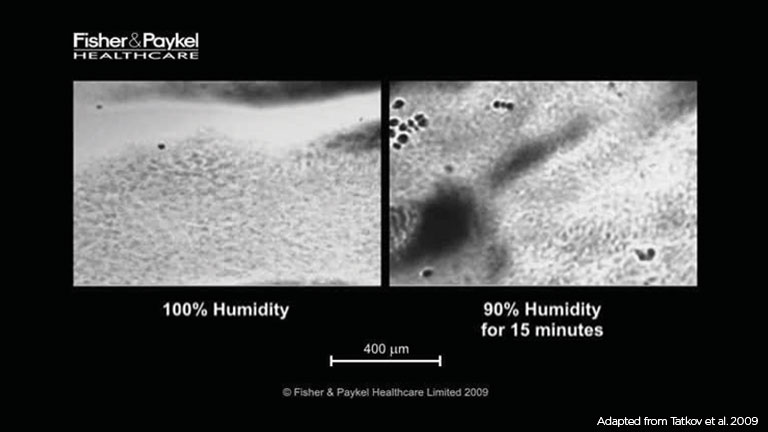
Image: healthy cilia beating to remove debris (e.g., bacteria) from the airway.
Watch this effect in action.
Watch the effect of low humidity under a microscope (1 min - turn audio on)
As the clip starts, you can see cilia beating. The dark spots moving across the left panel are debris (possibly bacteria) removed by effective mucociliary transport.
Conversely, debris in the right low-humidity panel stops as cilia slow, the effect of low humidity. After just an hour at 90% RH, the mucosa has dried out.
Do you need a refresher on how MCT works - watch this cool animation!

Patient comfort
Clinical evidence suggests that Optiflow NHF therapy provides better comfort than conventional oxygen delivery devices.10,11
Patients can eat, drink and sleep with the Optiflow interface and can more easily communicate with clinicians and families than with a mask.
Additionally, a study in JAMA12 found significantly reduced skin breakdown and noted a lower nurse workload with Optiflow NHF therapy compared with Bi-level ventilation.
Oxygen delivered via conventional oxygen therapy (COT) is 'bone' dry. Delivering oxygen via NHF therapy allows for oxygen to be optimally humidified eliminating the issues associated with exposure of the vulnerable upper airway to dry gas. Additionally delivering oxygen via NHF gives you confidence in the accurate delivery of blended oxygen.
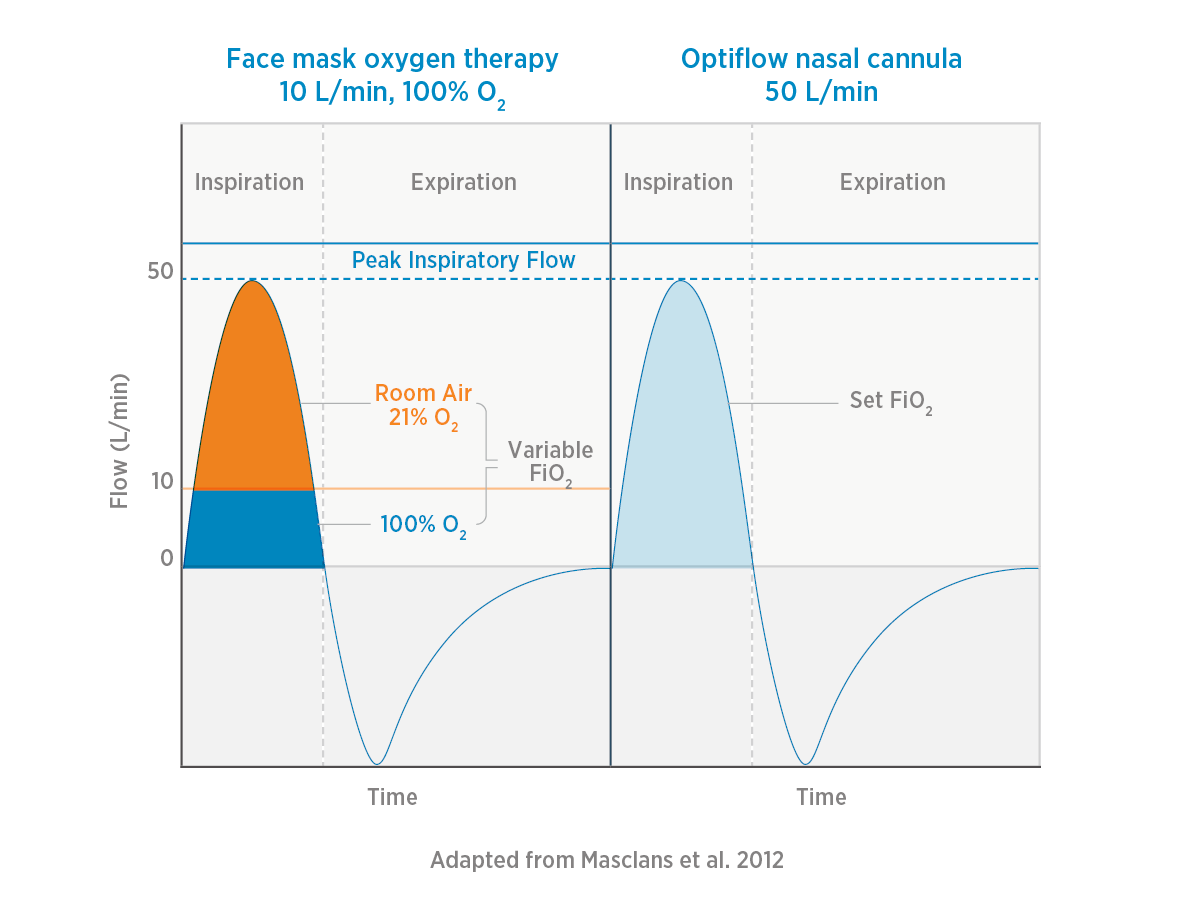
The advantage of NHF for oxygen delivery - is reducing oxygen dilution.
In the example illustrated, the maximum oxygen flow from the face mask (in the left panel) is limited to 10 L/min, which is insufficient to meet the patient’s peak inspiratory demand of 50 L/min.
The patient will draw in/entrain 40 L/min of room air to compensate, diluting the 100% oxygen delivered via the face mask.
Conversely, in the right panel, NHF therapy can meet the patient’s total inspiratory demand of 50 L/min without the need for dilution of oxygen - this gives confidence in the delivery of a specified FiO2.
Why using NHF gives you confidence in the oxygen fraction you are delivering.
With conventional oxygen, inspiratory flow is variable, so the oxygen fraction delivered is variable.
In contrast with NHF, you may be able to meet or exceed peak inspiratory flow, reducing or eliminating dilution from room air.
DPM-155